
In some studies, candiduria is even differentially defined for women and men. Even in adults, CFU criteria to diagnose candiduria range from 10 3 to 10 5 CFU/mL. Of concern is that neither the diagnostic criterion of colony forming unity (CFU) cutoff nor the collection technique (suprapubic aspiration versus bag collection) for neonatal urinary candidiasis is standardized. Although most studies rely on culture, both urine microscopic visualization and culture of urine could be employed. The definition of candiduria is enigmatic. Autopsy studies have noted renal cortical micro abscesses in most patients who have died of invasive candidiasis. Candida penetrates in the proximal tubules after passing by glomeruli and is eliminated in urine within weeks.
On the other hand, the hematogenous route is the way that the most kidney infection occurs in physiological state. The presence of an indwelling catheter allows biofilm formation and the persistence of the organism. The yeasts adhere to endothelial or urothelial cells, colonize the local area, evade the immune response, and, lastly, invade tissue or disseminate to distant sites within the body. The ascending infection of the upper urinary tract is rare, and the risk increases with obstruction of it, diabetes mellitus, or urinary reflux. By the ascending route, fungi are suggestively derived from the perineum, spreading into the bladder and then leading to colonization (it can occur into the collecting system of the kidneys). Urinary infections by Candida (usually asymptomatic) are caused by either the ascending or the hematogenous routes. and some aspects related to the immune response in fungal UTI, in addition to urinalysis perspectives in this clinical condition. This work explains the urinary findings and clinical picture of patients with fungal UTI caused by Candida spp. Leukocyturia is a cardinal sign of UTI caused both by bacteria or fungi and also is a key sign of the immune response occurring in the urinary tract when the organism faces an UTI. The detection and identification of fungi in urine samples (by microscopy and culture) plays an essential role in the diagnosis of fungal UTI.

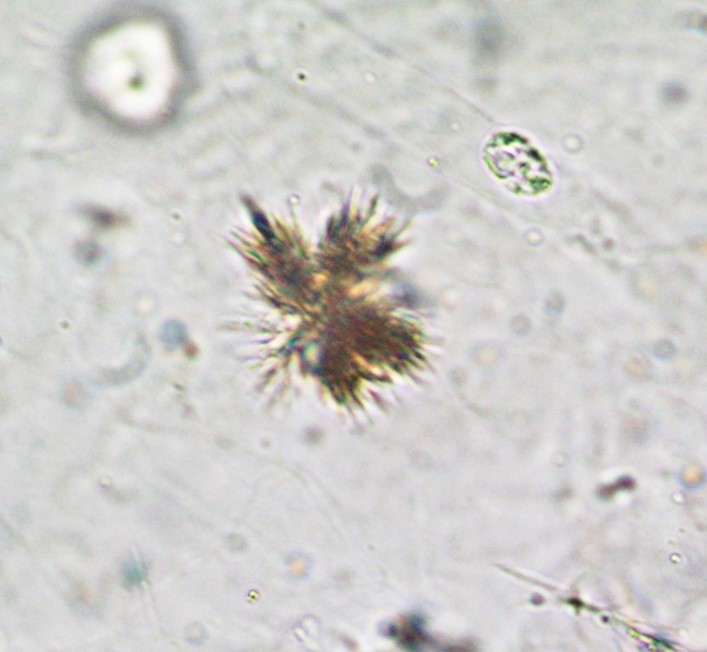
Non-yeast fungi, like some members of the Aspergillus, Mucorales, Blastomyces, and Histoplasma families, can also cause infections, especially among immunocompromised patients. Besides Candida, other agents, such as Cryptococcus spp., can cause UTIs. Fungi are pathogenic agents that can also cause disseminated infections involving the kidneys. This work explores the manifestations associated with the fungal UTI from the urinalysis perspective, namely the urinary findings and clinical picture of patients with fungal UTI caused by Candida spp., aspects associated with the immune response, and the future perspectives of urinalysis in the diagnosis of this clinical condition.įungal urinary tract infection usually means urinary tract infection (UTI) caused by Candida species with special attention to Candida albicans as the major fungal infectious agent. Indeed, urine markers of the immune response (leukocytes), urine barriers of tissue protection (epithelial cells), and urine markers of kidney disease (urinary casts) can be found in urine samples. The sediment analysis plays a key role in the identification of fungal UTI because both yeasts and pseudohyphae are easily identified and can be used as a clinical sign of fungal UTI but should not be overinterpreted. However, variable cutoff definitions and unreliable culture techniques may skew analysis of the incidence and outcome of candiduria. can cause urinary tract infection (UTI), as well as other non-yeast fungi, especially among immunocompromised patients.

Besides Candida, other agents like Cryptococcus spp.


 0 kommentar(er)
0 kommentar(er)
